
What is it?
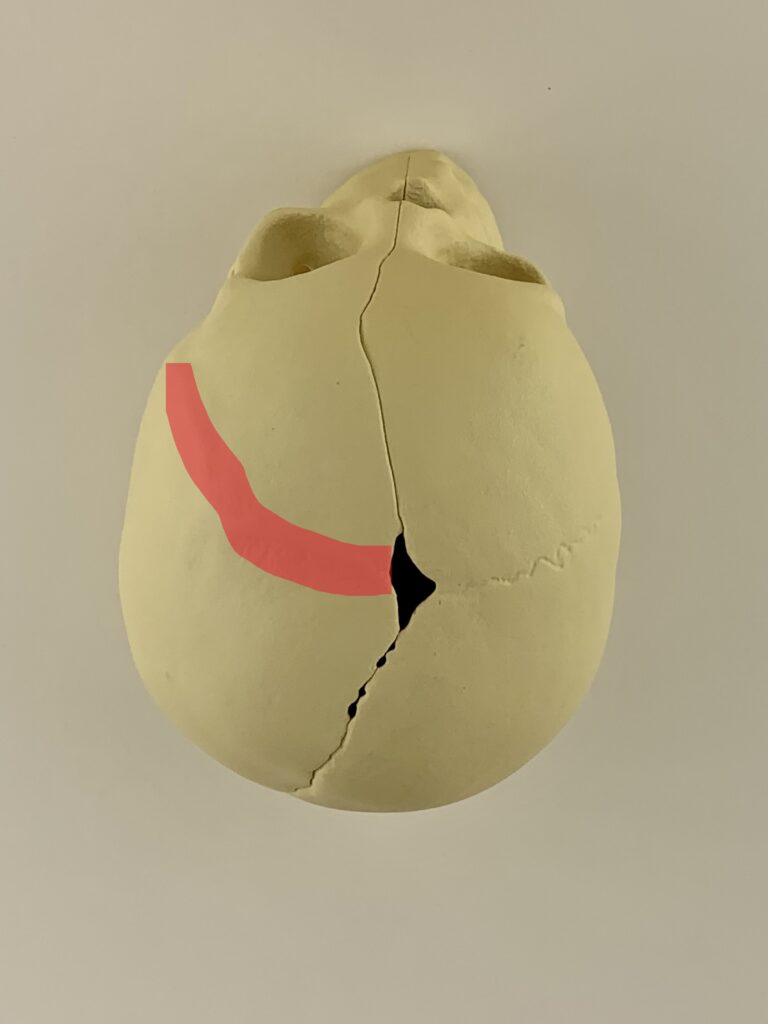
The coronal sutures are skull expansion joints running from side to side across the top of the skull, just behind the forehead. Unicoronal craniosynostosis is when one of these joints fuses prematurely (the left coronal suture is fused, shown in red in the skull model image below). When it prematurely fuses, the skull cannot grow the way it should as the brain grows. This causes an abnormally recessed and flattened forehead on the affected side.
What to look for?
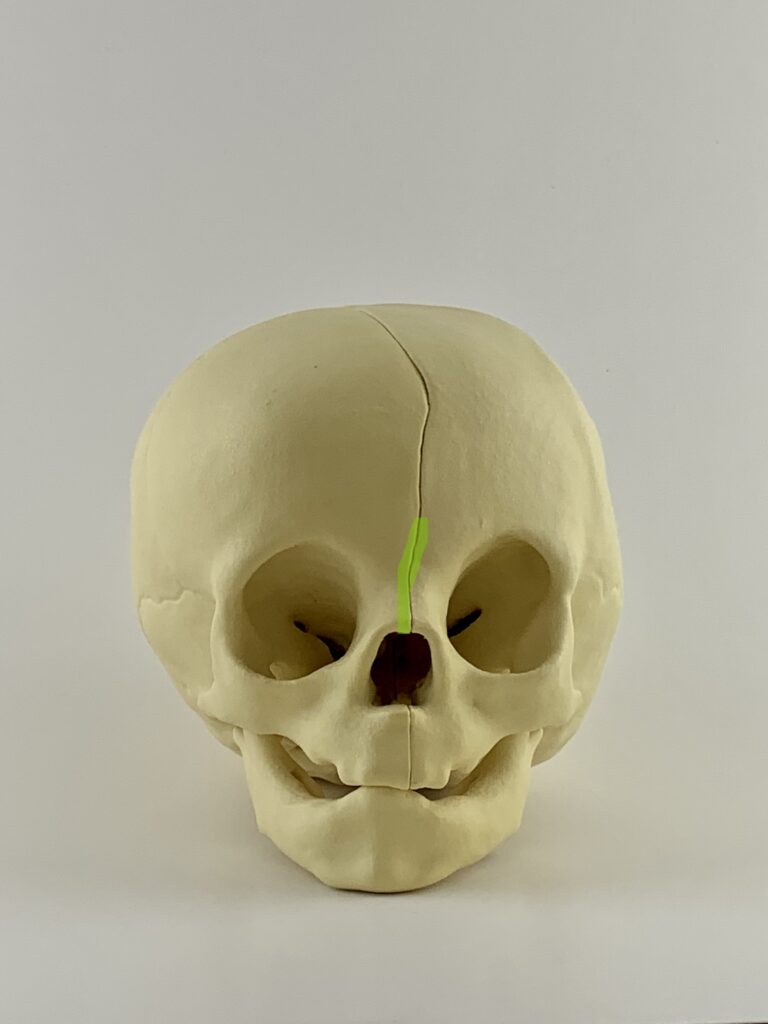
The forehead appears asymmetric, the affected side appears flat with an elevated eyebrow. The unaffected side appears prominent and round. The root of the nose can also deviate toward the fused suture (shown in green in the skull model image below).

Why is surgery recommended?
When the skull cannot grow as it should, it becomes progressively abnormal in appearance. Sometimes, intracranial pressure can become elevated. Surgery is recommended to normalize appearance, limit negative social interactions and reduce the risk of developmental concerns from elevated pressure.
Why is surgery recommended?
When the skull cannot grow the way it should, it becomes progressively abnormal in appearance. Sometimes, intracranial pressure can become elevated. Surgery is recommended to normalize appearance, limit negative social interactions and reduce the risk of developmental concerns from elevated pressure.
Before and After Cranioplasty Surgery




Frequently Asked Questions
The skull sutures can be thought of as expansion joints. These expansion joints play a critical role in allowing the skull to grow quickly when the brain is growing rapidly in the first 12 to 18 months of life. When one of these expansion joints fuses, this restricts growth in the direction perpendicular to the suture. When one of the coronal sutures is involved, the forehead on the side with the fused suture cannot grow forward and down as it wants to. The forehead assumes a flattened, recessed appearance on the side of the fused suture. However, the brain wants to find a way to grow, and so it pushes the normal side forward and down more. This makes the side with the normal suture look too round and sometimes makes the eye on that side look too small or as though it is closed too much. Sometimes, providers and parents alike assume the side of the forehead that appears prominent and rounded is the affected side, but it is the flattened, recessed side where the suture is fused.
There are 2 surgical approaches to treating unicoronal craniosynostosis – a minimally invasive approach and a traditional open surgical approach. For infants who are less than 5 months of age whose skull bones are very soft, we can use a minimally invasive approach. With minimally invasive surgery, small incisions are made at several key points along the top of the scalp. Working through those small incisions, the fused coronal suture is completely removed from the soft spot to a point just in front of the ear. We then use a postoperative molding helmet to fine-tune the head shape for a few months after surgery. For children who are older than 5 months whose bones are more dense, a traditional open approach is often required. With the traditional open approach, an incision is made over the top of the scalp from one ear to the other. The forehead bones as well as some of the bones of the orbit are removed, and a craniofacial surgeon will reshape the bones and move them forward to give a smooth, balanced forehead appearance and to make more space for the brain. While this surgery is a bigger operation, there is no need for molding helmet therapy after surgery in most cases.
The craniofacial plastic surgeon has specialized training in reconstructing and reshaping the skull and facial bones. The primary role of the craniofacial plastic surgeon is to assess the skull shape, determine the best way to normalize the shape and then perform the reconstruction to ensure the desired final result.
While it is the craniofacial plastic surgeon’s ultimate responsibility to reconstruct the head shape and give an excellent end result, it is also important to ensure that the fused suture and deformed skull bone be removed safely, taking care to protect the underlying brain and the dura, the lining around the brain. For this reason, we always partner with a pediatric neurosurgeon whose primary role is to protect the brain and ensure the safe removal of bone to facilitate craniofacial surgeon’s reconstruction.
For over 25 years, we have been loyal partners of St. Luke’s Children’s Hospital in Boise, Idaho in caring for children with complex pediatric cleft and craniofacial problems. We have always felt that pediatric surgical care should be offered in the setting where dedicated, fellowship trained pediatric anesthesia specialists are available to ensure the safest possible surgery for the children that we care for.
The timing of surgery for craniosynostosis can vary depending on how old your child is at the time of diagnosis, their overall health and the surgical approach selected by you and your craniofacial surgeon. If your child is healthy and is diagnosed at an early age (in the first 2-3 months of life), then minimally invasive surgery can often be done between 2-5 months of age. If your child is diagnosed at a later age (after 5 months) or needs an open surgical approach or has health concerns that require waiting to perform surgery until they are older, your child’s surgery may be done closer 9-12 months of age.
